
ISSN: 3080-1427 (online) / 3080-1419 (print)
Volume 1, Issue 4 (October 2025 – December 2025), pp: 1-5
![]()
Bone Marrow Transplantation in a Young Adult with Acute Myeloid Leukemia: A Case Report
Bestoon S. Hasan 1,a*, Hardee J. Saber 2,b
1 Awat Radiation Oncology Center, Erbil, Iraq.
2 Nanakali Teaching Hospital, Erbil, Iraq.
E-mail: dr.bestoon@hotmail.com a,*, Hardee1@gmail.com b
Received: 05 July 2025 | Revised: 10 August 2025 | Accepted: 12 September 2025 | Published: 05 October 2025
Acute myeloid leukemia (AML) is a rapidly progressing blood cancer. For suitable candidates, allogeneic hematopoietic stem cell transplantation (allo HSCT) offers a potential cure, albeit with serious risks, notably graft-versus-host disease (GVHD). We hereby present a case of a 31-year-old male patient diagnosed with intermediate-risk acute myeloid leukemia (AML) according to the 2017 European Leukemia Net (ELN) classification who underwent allogeneic hematopoietic stem cell transplantation (allo-HSCT) and subsequently developed grade III gastrointestinal and liver graft-versus-host disease (GVHD). This report underscores the imperative for early detection, targeted immunosuppression, and ongoing post-transplant monitoring to avert life-threatening consequences. The patient demonstrated a complete recovery, devoid of chronic GVHD, thereby substantiating the efficacy of prompt intervention and multidisciplinary care.
Keywords: Acute Myeloid Leukemia, Allogeneic Hematopoietic Stem Cell Transplantation, Graft-versus-Host Disease, Liver Dysfunction, Post-transplant Complications.
Acute myeloid leukemia (AML) encompasses a range of genetic and epigenetic abnormalities, resulting in uncontrolled proliferation of immature myeloid cells and bone marrow failure (Döhner et al., 2015; Kantarjian et al., 2024). Although standard intensive chemotherapy can induce remission, relapse rates—especially in cases with high-risk molecular markers—are a source of concern (DiNardo et al., 2023; Wachter & Pikman, 2024). Allogeneic hematopoietic stem cell transplantation (allo-HSCT) remains the most robust curative option, leveraging both cytotoxic therapy and graft-versus-leukemia effects (Appelbaum, 2007; Chen et al., 2023; Copelan, 2006; Thomas et al., 1979). Despite the strides made in the field of medicine, acute GVHD continues to be a major cause of morbidity and mortality following transplantation procedures. This underscores the importance of early recognition and prompt intervention in determining patient outcomes.
This report delineates a clinical case of a 31-year-old male diagnosed with AML who was managed with allo-HSCT, with a focus on the treatment trajectory, encountered complications, and subsequent outcomes.
The patient’s preliminary laboratory evaluation revealed significant pancytopenia and abnormal liver function tests. A comprehensive summary of the findings is provided in Table 1.
Table 1. Laboratory Test Results
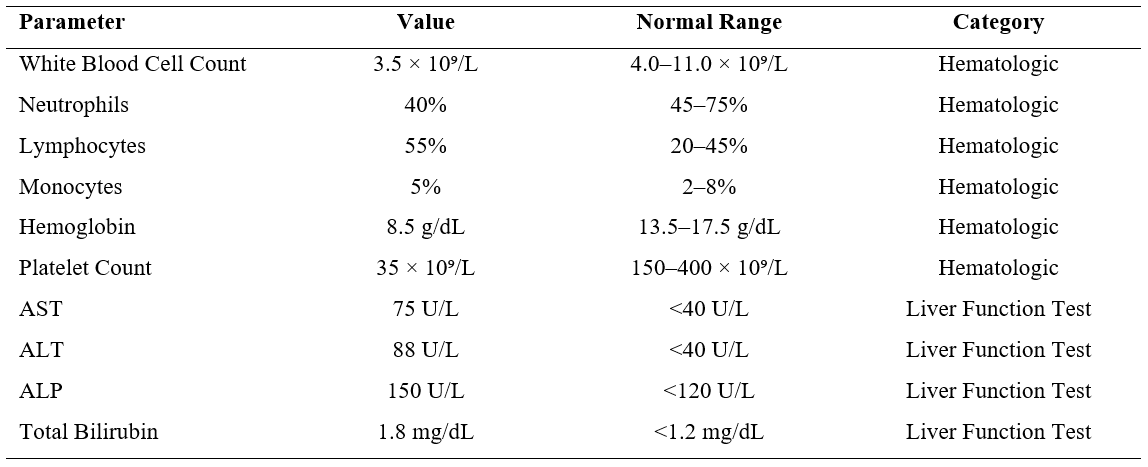
A bone marrow biopsy was conducted, and the results indicated an intermediate-risk acute myeloid leukemia (AML) according to the 2017 European Leukemia Net (ELN) risk stratification system (Döhner et al., 2017). The presence of an NPM1 mutation and the absence of FLT3-ITD were also noted, along with the presence of CD34/CD33-positive myeloblasts.
Following induction (7+3) and consolidation with high-dose cytarabine, complete remission was achieved. However, mild elevations in liver enzymes were observed during the course of therapy, which resolved with the administration of supportive care. Given the patient’s profile and the risk of relapse, the treatment team pursued allo HSCT from a matched unrelated donor (Cornelissen & Blaise, 2016; Inoue et al., 2025; Li & Zhou, 2023). A matched sibling donor was not available, and a matched unrelated donor (MUD) was selected based on HLA compatibility and a favorable donor-recipient risk profile. The patient underwent a series of pre-transplant procedures, including the administration of busulfan and cyclophosphamide. Liver enzymes were meticulously monitored due to preexisting hepatic concerns. The prophylaxis for GVHD consisted of cyclosporine and methotrexate. Neutrophil engraftment occurred at day +18, with 98% donor chimerism by day +30. However, a subsequent increase in liver enzyme levels was observed.
By day +25, the patient’s total bilirubin level increased to 4.2 mg/dL, aspartate transaminase (AST)/alanine transaminase (ALT) levels rose to approximately 250–300 U/L, and ultrasound imaging revealed hepatic venous congestion, raising concern for veno-occlusive disease (VOD) and/or sinusoidal obstruction syndrome (SOS). A liver biopsy was deemed contraindicated due to thrombocytopenia. By day +35, the patient exhibited symptoms of severe diarrhea and abdominal pain, accompanied by further elevated levels of bilirubin and ALP. GI endoscopy and histology confirmed grade III GI GVHD (Ferrara et al., 2009; Holler et al., 2024), while liver involvement (stage 2) was diagnosed based on biochemical criteria and correlated with Glucksberg staging (Justiz Vaillant et al., 2025).
The patient was administered a high-dose of methylprednisolone (2 mg/kg/day), which led to a partial response in the patient’s gastrointestinal symptoms. Liver enzymes and bilirubin reached their maximum levels on approximately day +40, with values of ~12 mg/dL. The administration of ATG was necessitated by an inadequate response to steroids. The therapeutic interventions administered included intravenous fluids, electrolytes, total parenteral nutrition (TPN), transfusions, analgesic treatment, cyclosporine level adjustment, coagulation support, and nutritional support from a registered dietitian.
The patient exhibited complications, including febrile neutropenia with Pseudomonas aeruginosa bacteremia, necessitating meropenem treatment. Meticulous fluid and nutrition management was imperative due to underlying liver dysfunction. Over the course of subsequent weeks, the symptoms associated with GVHD diminished; bilirubin levels returned to normal by day +90, although transaminases persisted at a slightly elevated state for an extended duration. The administration of steroids and immunosuppressants was systematically reduced. At one year post-transplant, the patient was in remission with full functional recovery, normal liver function, and no chronic GVHD. A long-term care plan was implemented, including monitoring for secondary malignancies, endocrine issues, cataracts, and mental health support (Bauchat et al., 2025; Feldt-Rasmussen & Klose, 2000).
The study protocol received ethical clearance from the institutional review boards of all participating oncology centers. In accordance with the principles of confidentiality and ethical standards, all patient data were anonymized.
This case underscores the curative promise and hazards of allo-HSCT in intermediate-risk AML (Appelbaum, 2007; Copelan, 2006; Cornelissen & Blaise, 2016; Yang et al., 2022). While pre-transplant hepatic testing provided an initial safety check, underlying liver vulnerability emerged post-transplant, highlighting the limits of tools like the HCT-CI (Abdelbary et al., 2020). Graft-versus-host disease (GVHD), particularly its acute gastrointestinal and hepatic manifestations, continues to be the foremost post-transplant complication (Ferrara et al., 2009; Zeiser & Blazar, 2017). A meticulous clinical and histopathologic assessment is imperative for prompt differentiation from other etiologies, such as VOD, drug-induced liver injury, or viral hepatitis. This assessment is occasionally constrained by the risk of bleeding (Colecchia et al., 2019). In this particular instance, the gastrointestinal and hepatic manifestations corresponded to stage 2 and grade III GVHD according to the Glucksberg criteria (Justiz Vaillant et al., 2025; Smallbone et al., 2025). The onset of GVHD is characterized by the recognition of host tissues by donor T cells as foreign, thereby inducing an inflammatory response that results in tissue damage (Socie & Michonneau, 2022). The administration of corticosteroids in the early stages of the condition is of paramount importance (Cooper & Abkowitz, 2023). In cases that are steroid-refractory, such as the present one, the addition of agents such as ATG, ruxolitinib, or ECP is supported by recent literature (Solh et al., 2023; Zeiser & Blazar, 2017). In our case, ATG was selected based on institutional protocol, prior experience, and the patient’s immunological profile. However, ruxolitinib and ECP remain viable alternatives supported by recent guidelines. Optimal management necessitates an integrated approach to fluid status, electrolytes, nutrition, infection prevention, and drug dose adjustments, particularly when liver function is compromised. The involvement of a multidisciplinary care team is imperative. The positive outcome, characterized by prolonged remission and organ recovery, underscores the efficacy of meticulous, collaborative GVHD management. Long-term monitoring remains pivotal to the detection of chronic GVHD, second cancers, endocrine dysfunction, ocular issues, and psychological sequelae (Arai et al., 2015; Bauchat et al., 2025).
This young man’s case exemplifies the potential of allogeneic hematopoietic cell transplantation (allo-HSCT) to cure, which is counterbalanced by its risks, notably acute graft-versus-host disease (GVHD) in the gastrointestinal tract and the liver. The patient’s recovery was facilitated by an early diagnosis, the administration of aggressive immunosuppressive therapy, and the provision of sustained multidisciplinary support. It is imperative to acknowledge the necessity of sustained post-transplant vigilance in ensuring the preservation of long-term function and survival in patients diagnosed with acute myeloid leukemia (AML) who are undergoing allohematopoietic stem cell transplantation (allo HSCT). Multidisciplinary care teams have been shown to play a vital role in improving outcomes by ensuring the coordinated management of complications, such as acute GVHD.
The study protocol received ethical clearance from the institutional review boards of all participating oncology centers. In accordance with the principles of confidentiality and ethical standards, all patient data were anonymized.
Not applicable.
The data that supports the findings of this study are available from the corresponding author upon reasonable request.
The authors declare that there are no conflicts of interest.
The authors declare that this research received no external funding.
B.S.H: Conceptualization, Resources, Writing of the original draft, Writing – review & editing, Project adminstration.
H.J.S: Conceptualization, Writing of the original draft, Writing – review & editing.
Not applicable
The authors declare that no generative AI or AI-assisted technologies were used in the preparation of this work.
Cite: Hasan, B. S., & Saber, H. J. (2025). Bone Marrow Transplantation in a Young Adult with Acute Myeloid Leukemia: A Case Report. Middle Eastern Cancer and Oncology Journal, 1(4), 1–5. https://doi.org/10.61706/MECOJ160173
Copyright: © 2025 by the authors. Licensee Scientific Steps International Publishing Services, Dubai, UAE.
This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).



An independent academic publisher with an editorial team including many of the top researchers in the world. SSG publishes research, review, and case report articles in double-blind, peer-reviewed, open access scientific and academic journals.
Copyright © 2025 Scientific Steps International Publishing Services LLC (Dubai – United Arab Emirates)